Research
Arterial spin labeled (ASL) perfusion MRI
Arterial spin labeling (ASL) uses magnetic labeling of endogenous blood water as a diffusible tracer for quantification of tissue perfusion in classical units of m/g/min. Dr. Detre is a co-inventor of ASL MRI and has been involved in its development, validation, and applications for over two decades. Current technical development work focuses on increasing the spatial and temporal resolution of ASL MRI through the use of parallel imaging methods, on the development of ultra-high-field ASL MRI for studying weakly perfused tissues, and on the development of signal processing strategies to improve the reliability of CBF measures derived from ASL MRI. This work is primarily supported through a NIH Regional Resource for magnetic resonance and optical methods.
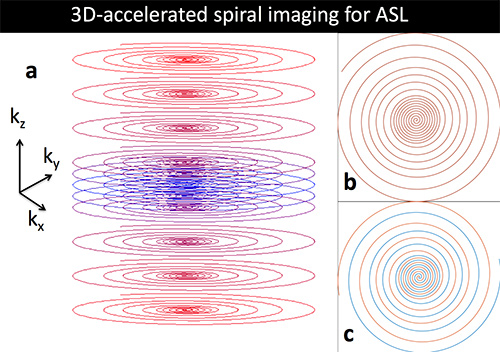
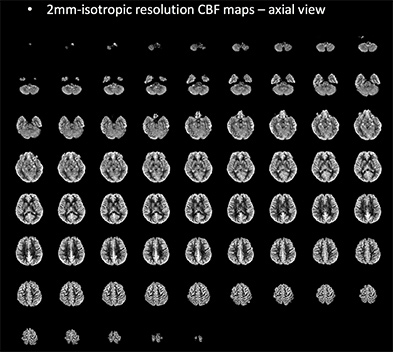
Perfusion MRI for multisite studies of brain function
Arterial Spin Labeled (ASL) perfusion MRI provides noninvasive quantification of cerebral blood flow (CBF), which is a versatile biomarker of brain function. ASL is one of the few MRI contrast mechanisms whose physiological basis is well known. Further, because ASL MRI provides absolute quantification of a physiological parameter, it should be ideally suited for multisite studies measuring brain function across multiple MRI platforms and across time. This project carried out in collaboration with David Alsop at Harvard seeks to optimize ASL MRI methods for cross-platform studies of drug actions on the brain by further characterizing sources of variance in ASL MRI data and through validation studies using pharmacological modulation of regional brain function.
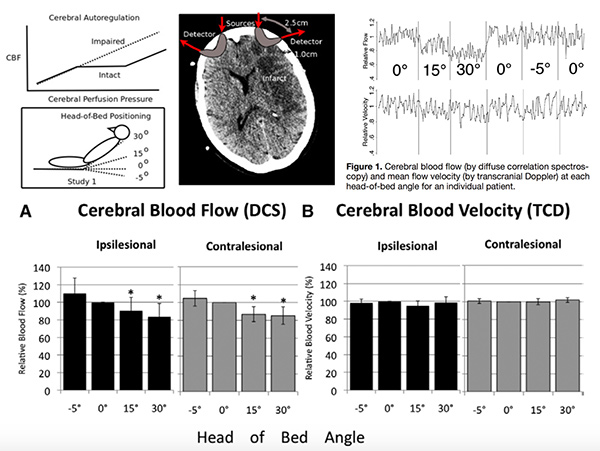
Diffuse optics for acute stroke management
Diffuse correlation spectroscopy is an optical method for noninvasively monitoring cerebral blood flow (CBF) developed by Arjun Yodh and colleagues in the Department of Physics at Penn, and is suitable for use at the bedside to monitor CBF in patients. Hypoperfusion is the proximate cause of stroke, and nearly all therapies used in stroke management are intended to optimize brain perfusion, yet CBF is rarely if ever measures in patients with stroke. An NIH Bioengineering Research Partnership supports both methodological development and clinical translation of diffuse correlation spectroscopy for use in stroke care. Dr. Detre leads the clinical component of this project, which also includes collaborators from the Penn Stroke Center.
The Human Placenta Project
The placenta is an underserved organ! The Human Placenta Project is a collaborative research effort, launched by the National Institute of Child Health and Development, to understand the role of the placenta in health and disease. The placenta is the least understood human organ but arguably one of the most important. It influences not just the health of a woman and her fetus during pregnancy, but also the lifelong health of both. The University of Pennsylvania is participating in the Human Placenta Project (PIs Nadav Schwartz and Daniel Licht) and our role is to develop MRI based flow and perfusion imaging of the human placenta.
Collaborative Research
Glutamate imaging with MRI
Glutamate is the most abundant neurotransmitter in the brain and also a key metabolic intermediate. Total brain glutamate can be quantified by magnetic resonance spectroscopy (MRS) and now imaged at ultra-high magnetic field using a novel approach based on chemical exchange saturation transfer, termed GluCEST. In collaboration with Ravinder Reddy and the Penn Center for Magnetic Resonance and Optical Imaging we are developing applications of GluCEST as a biomarker of brain function, including studies in epilepsy and neurodegenerative diseases.
Neuroimaging in Epilepsy
Epilepsy is a common and frequently disabling neurological disorder affecting almost 1% of the adult population and a higher proportion of children. While some epilepsy is due to genetic defects affecting the entire brain, many cases of epilepsy are “localization related” and thought to arise from a focal lesion, often in the mesial temporal lobe. Epilepsy can be treated surgically if the lesion can be identified, however, only a fraction of epileptic lesions are visible using conventional structural MRI. Our lab has pioneered the use of functional MRI to visualize seizures and the use of fMRI with memory tasks to evaluate mesial temporal lobe function. Most recently, we are assessing GluCEST as a biomarker of epileptogenic cortex. This work is now carried out in collaboration with Kathryn Davis and the Penn Epilepsy Center.
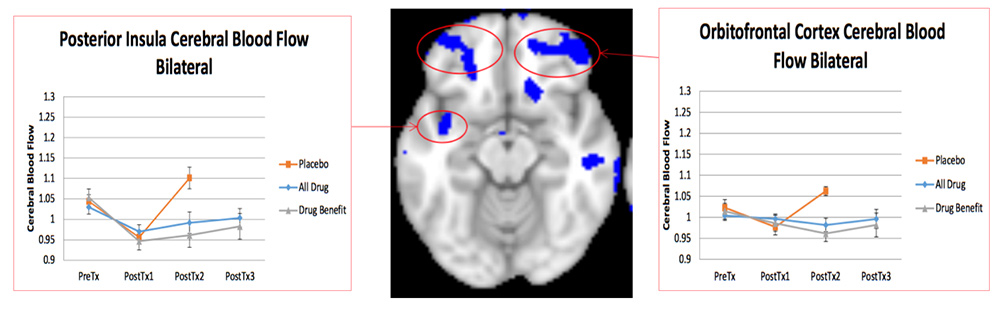
Neuroimaging in Smoking and Drug Addiction
Drug addiction and drug abstinence is associated with changes in regional brain function that may hold the key to successful treatment. Arterial spin labeled (ASL) perfusion MRI provides a means of quantifying brain “states” and can be used to study changes in regional brain function during abstinence and drug craving states. We have a longstanding collaboration with AnnaRose Childress and Teri Franklin at Penn’s Center for Studies of Addiction to apply this technology to drug addiction research.
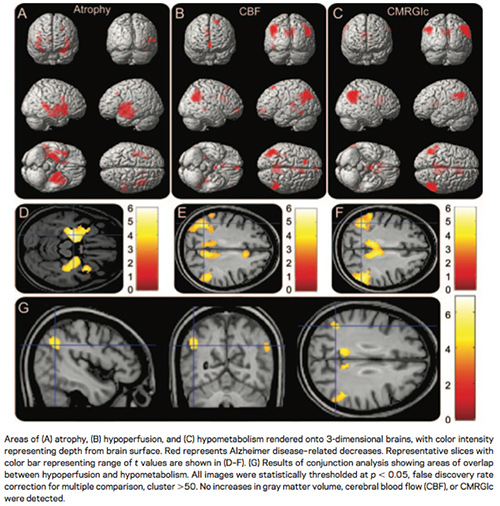
Biomarkers of Neurodegeneration
Alzheimer’s disease and other neurodegenerative disorders are responsible for much of age related cognitive decline, and are an increasing public health concern as the population ages. The development and validation of brain biomarkers of neurodegeneration is an important component of research aimed as developing treatments for these disorders. It is hoped that disease biomarkers will allow earlier identification of neurodegenerative pathologies, and provide a more sensitive measure of treatment effects, than clinical symptoms. In collaboration with David Wolk at the Penn Memory Center and Murray Grossman at the Penn FTD Center, we have pioneered the use of arterial spin labeled (ASL) perfusion MRI as a biomarker of regional neurodegeneration. This work has led to the incorporation of ASL MRI in the Alzheimer’s Disease Neuroimaging Initiative. We also collaborate with Paul Yushkevich in the Department of Radiology on MRI based morphemetry of the hippocampus.
Neural Correlates of Sleep and Sleep Deprivation
Sleep is critically important for health and sleep deprivation, though endemic in modern society, is associated with adverse effects on health and cognition. In collaboration with David Dinges and Hengyi Rao at Penn’s Center for Sleep and Circadian Neurobiology, we are using multimodal MRI to study the neural correlates of sleep deprivation. We are also collaborating with Max Kelz to study the neurological correlates of pharmacologically induced sleep, with a focus on attempting to identify sleep associated changes in brain glymphatic function. A related project in collaboration with the Wehrli lab concerns the neurometabolic correlates of obstructive sleep apnea.
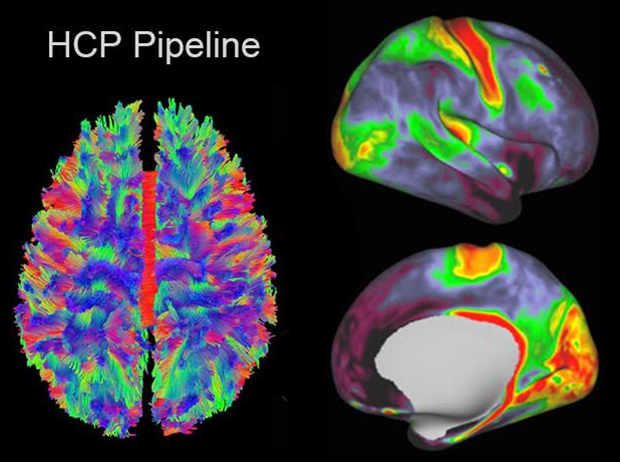
Brain Connectomes in Disease
Magnetic resonance neuroimaging now provides unprecedented opportunities to map connectivity in the living human brain, leveraging diffusion tensor imaging based tract tracing and resting state functional MRI based correlations between brain regions. The NIH funded Human Connectome Project has developed the framework for applying advanced connectomics to study connectivity in the normal human brain, and a related initiative will apply these methods to brain disorders. Our lab is participating in projects aimed at mapping connectivity changes in frontotemporal dementia (PI Murray Grossman and the Penn FTD Center) and in anxious misery (PI Yvette Sheline and the Penn Center for Neuromodulation in Depression and Stress.
Neural Correlates of Pain
Pain is the most common reason for seeking medical care, yet the neural basis of acute and chronic pain and its treatment are incompletely understood. While fMRI has been used extensively to study the neural correlates of evoked pain, arterial spin labeled (ASL) perfusion MRI allows the neural correlates of painful states and their treatment to be studies without additional noxious stimuli. We are collaborating with John Farrar in Anesthesiology and Elliott Hersh in Dental Medicine on the neural correlates of dental pain, and with Lily Arya in Urology on bladder pain.
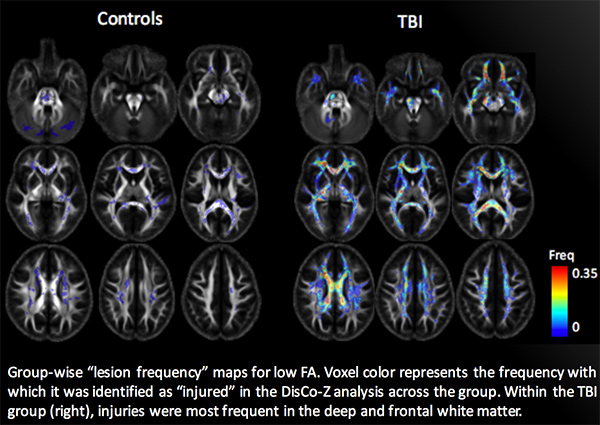
Traumatic Brain Injury
Both mild and severe traumatic brain injury (TBI) can result in long-term cognitive deficits, even in the absence of structural lesions on conventional brain imaging. We have a longstanding collaboration with Hoon Kim and John Whyte at the Moss Rehabilitation Research Institute (http://mrri.org) to use advanced MRI methods to study the neural correlates of attentional deficits after moderate TBI. Most recently we have been collaborating with Amanda Rabinowitz and Douglas Smith at Penn’s Center for Brain Injury and Repair on the neural correlates of cognitive deficits following mild TBI.